El microbioma uterino desempeña un papel crucial en la salud reproductiva y la fertilidad. Este complejo ecosistema de bacterias y microorganismos influye en la implantación, el éxito del embarazo y el bienestar ginecológico general. Las investigaciones sugieren que los desequilibrios del microbioma uterino pueden contribuir a la infertilidad, al fallo recurrente de implantación en la FIV y a afecciones como la endometriosis. Comprender cómo afecta el microbioma uterino a la fertilidad y aprender formas de optimizarlo puede ser valioso para las personas que quieren quedarse embarazadas.
¿Qué es el microbioma uterino?
El microbioma uterino está formado por bacterias y otros microorganismos que residen en el revestimiento endometrial. Esta comunidad microbiana varía en función de factores como la edad, los cambios hormonales, la etnia y el uso de anticonceptivos, sobre todo dispositivos intrauterinos (DIU).
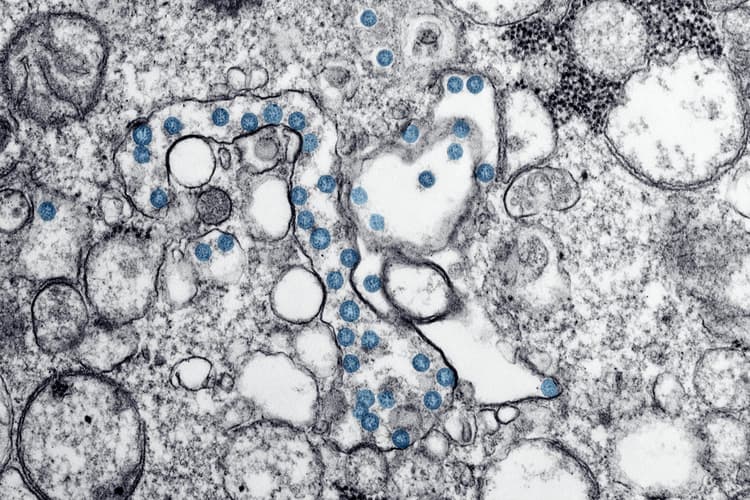
Un microbioma endometrial equilibrado suele ser rico en especies de Lactobacillus, que se asocian a una función reproductora sana. Sin embargo, se produce un desequilibrio -denominado disbiosis- cuando otras bacterias, como Streptococcus, Prevotella, Gardnerella y Atopobium, se vuelven dominantes. Estos cambios pueden estar relacionados con problemas de salud reproductiva y ginecológica, como se destaca en investigación publicada en la Biblioteca Nacional de Medicina.
Por qué es importante el microbioma uterino
La investigación ha puesto cada vez más de relieve la conexión entre el microbioma uterino y diversos aspectos de la salud reproductiva, entre ellos:
- Fertilidad: Un microbioma endometrial desequilibrado se ha asociado a fallos recurrentes de implantación en los tratamientos de FIV, mientras que un microbioma bien equilibrado se correlaciona con mayores tasas de éxito en los resultados del embarazo, según un estudio publicado en Nature.
- Endometriosis: Estudios en curso sugieren que los desequilibrios microbianos en el útero pueden contribuir a la inflamación y la desregulación del sistema inmunitario asociadas a la endometriosis.
- Salud reproductiva general: Un microbioma sano favorece la función inmunitaria y ayuda a mantener un entorno uterino estable, reduciendo la inflamación y el riesgo de infección, como se expone en un estudio de PubMed sobre salud reproductiva.
El vínculo entre los microbiomas uterino y vaginal
Los microorganismos que se encuentran en el microbioma uterino a menudo se solapan con los del microbioma vaginal, sobre todo en los casos de vaginosis bacteriana (VB). Puesto que los microbiomas reproductivos están interconectados, los desequilibrios en uno pueden influir en el otro.
Aunque la investigación en este campo está en curso, el análisis del microbioma uterino ofrece una nueva vía para comprender la salud reproductiva y optimizar los resultados de la fertilidad. Sin embargo, es importante señalar que esta prueba no es una herramienta diagnóstica, sino un método avanzado para evaluar el equilibrio microbiano.
Cómo mejorar el microbioma uterino
Mantener un microbioma uterino equilibrado es esencial para la salud reproductiva. Hay varias estrategias de estilo de vida y médicas que pueden ayudar a mantener un microbioma sano.
1. Probióticos y dieta
Una dieta rica en probióticos puede mejorar significativamente el equilibrio microbiano en el útero. Consumir alimentos ricos en probióticos, como yogur, kéfir, kimchi, chucrut y otras verduras fermentadas, ayuda a aumentar los niveles de Lactobacillus, que son beneficiosos para la salud reproductiva. Los alimentos prebióticos, como el ajo, las cebollas, los plátanos y los espárragos, también pueden favorecer el crecimiento de bacterias beneficiosas. En algunos casos, los profesionales sanitarios pueden recomendar suplementos probióticos específicamente diseñados para la salud vaginal y uterina.
2. Evitar antibióticos innecesarios
Aunque los antibióticos son esenciales para tratar las infecciones bacterianas, su uso excesivo puede provocar desequilibrios en el microbioma. Los antibióticos de amplio espectro pueden eliminar las bacterias beneficiosas, permitiendo que prosperen las dañinas. Si el uso de antibióticos es necesario, considera la posibilidad de hablar con un profesional sanitario sobre la suplementación con probióticos para restablecer el equilibrio microbiano. Siempre debes hablar con un profesional sanitario sobre el uso de antibióticos en general y no debes evitarlos sin la aprobación de tu médico.
3. Controlar el estrés
El estrés crónico puede afectar negativamente a la función inmunitaria y a la regulación hormonal, dos factores que influyen en el microbioma. Los niveles elevados de cortisol pueden contribuir a la inflamación, dificultando el desarrollo de las bacterias beneficiosas. Las técnicas de control del estrés, como la atención plena, el yoga, el ejercicio regular y un sueño adecuado, pueden contribuir tanto al bienestar mental como a la salud del microbioma.
4. Limitar las duchas vaginales y los productos de limpieza agresivos
El uso de duchas vaginales, jabones fuertes o productos de higiene femenina muy perfumados puede alterar el equilibrio natural de las bacterias en los entornos vaginal y uterino. El sistema reproductivo se limpia solo, y suele bastar con agua o jabón suave sin perfume para la limpieza externa. Evitar los productos de limpieza vaginal innecesarios ayuda a mantener un microbioma estable y reduce el riesgo de infecciones.
5. Buscar orientación médica
Para quienes tienen problemas de fertilidad o infecciones recurrentes, consultar a un especialista sobre las pruebas microbianas puede aportar información sobre los desequilibrios subyacentes. Las pruebas del microbioma uterino, ya sea mediante biopsias endometriales o análisis de sangre menstrual no invasivos, pueden ayudar a identificar disbiosis y orientar planes de tratamiento personalizados. En algunos casos, pueden ser necesarias intervenciones como la terapia probiótica, los antibióticos o la regulación hormonal para restablecer el equilibrio.
Cómo se analiza el microbioma uterino
El estudio de la composición del microbioma uterino es un campo de investigación emergente, y se han desarrollado diversos métodos de prueba para evaluar el equilibrio microbiano. Tradicionalmente, la forma más habitual de analizar el microbioma uterino ha sido mediante una biopsia endometrial. Sin embargo, este método es invasivo y no siempre resulta práctico para las pruebas rutinarias.
Análisis del microbioma de la sangre menstrual
Una alternativa menos invasiva a las biopsias son las pruebas del microbioma de la sangre menstrual, que permiten evaluar el entorno uterino mediante un sencillo proceso de recogida de muestras. La sangre menstrual contiene valiosa información microbiana que puede ofrecer información sobre el equilibrio de las bacterias presentes en el útero.
Las muestras pueden recogerse utilizando:
- Una copa menstrual
- Recogida directa de sangre menstrual
- Una torunda vaginal el primer día de la menstruación
En qué se diferencia el análisis de sangre menstrual del análisis del microbioma vaginal
Aunque los microbiomas vaginal y uterino son distintos, se influyen mutuamente. Muchas personas con desequilibrios en el microbioma vaginal pueden tener también desequilibrios en el microbioma uterino, y viceversa. Analizar ambos puede proporcionar una comprensión más completa de la salud reproductiva y de los posibles problemas de fertilidad.
El microbioma uterino y el éxito de la FIV
Para quienes se someten a tratamientos de fertilidad, es crucial comprender el papel del microbioma uterino en el éxito de la FIV. Los estudios indican que un microbioma óptimo, dominado por Lactobacillus, puede mejorar significativamente las tasas de implantación y los resultados del embarazo. Por el contrario, la presencia de bacterias patógenas se ha relacionado con fallos de implantación y abortos espontáneos.
Al abordar los desequilibrios microbianos antes de la FIV, las personas pueden aumentar sus posibilidades de éxito y mejorar su salud reproductiva general, como se destaca en investigación de la Biblioteca Nacional de Medicina.
Avanzar en la investigación sobre salud reproductiva
A medida que siguen evolucionando los estudios sobre el microbioma endometrial, los hallazgos sugieren que el equilibrio microbiano en el útero puede desempeñar un papel fundamental en la fertilidad, la endometriosis y la salud reproductiva en general. La investigación continua es esencial para comprender plenamente estas relaciones y mejorar la atención sanitaria femenina.
El creciente interés por las pruebas del microbioma de la sangre menstrual refleja un cambio importante hacia enfoques no invasivos de la salud reproductiva impulsados por la investigación. Al explorar este campo emergente, tanto las personas como los profesionales sanitarios pueden profundizar en las complejidades del microbioma femenino y su impacto en el bienestar.