¿Qué se mide en un análisis de semen masculino?
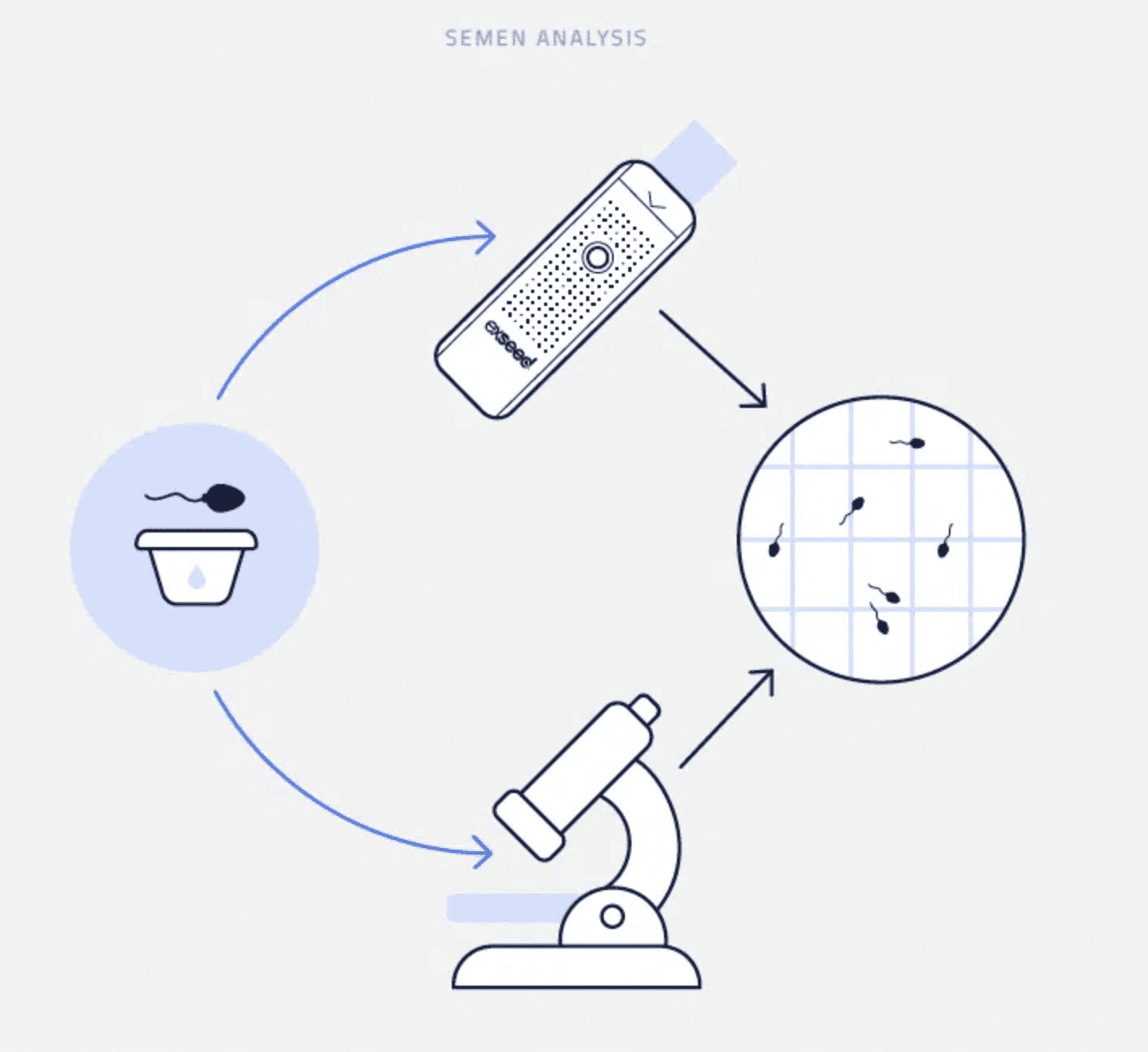
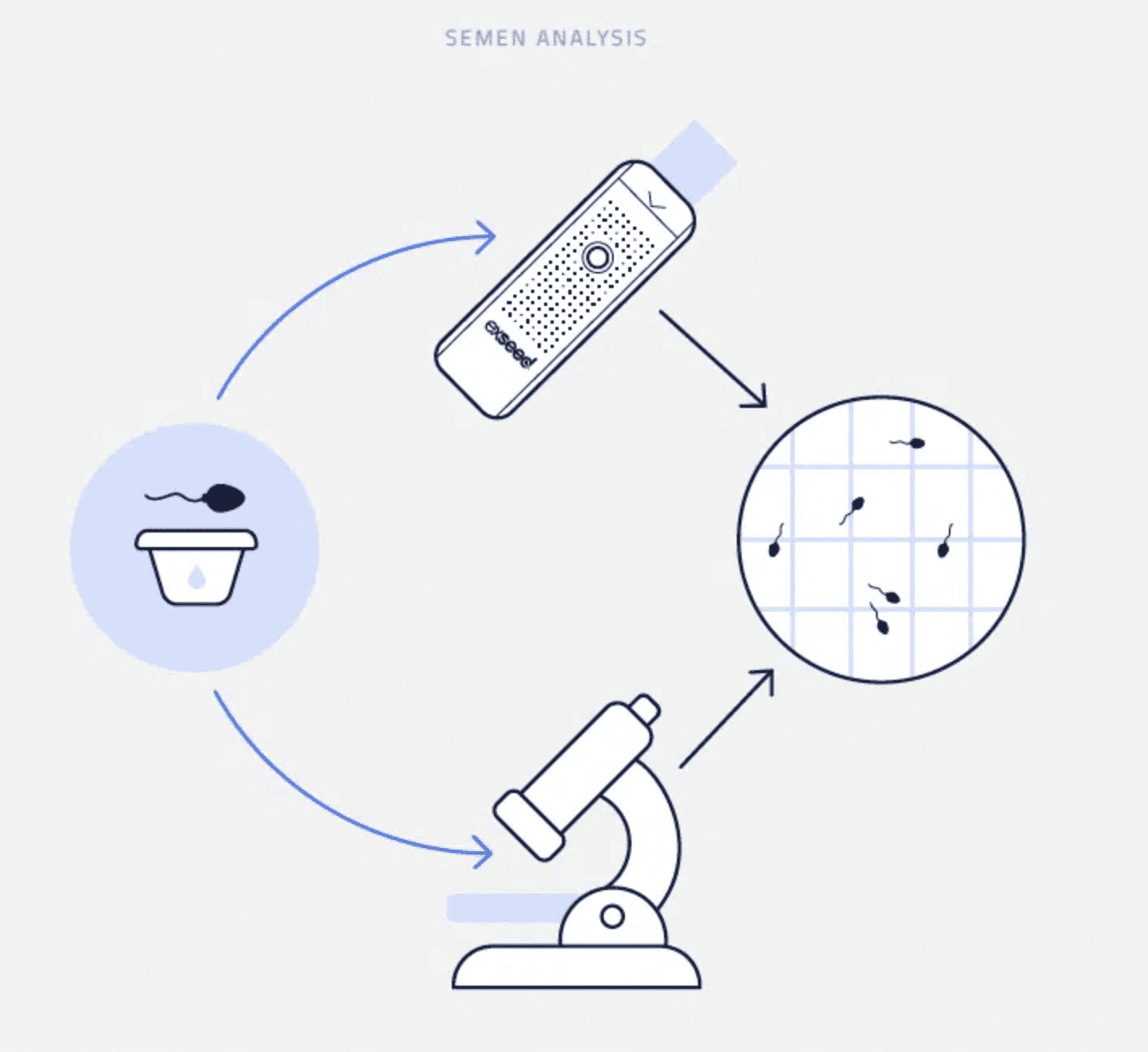
El semen es el líquido liberado durante la eyaculación, que contiene espermatozoides que fecundan el óvulo. En un análisis de semen estándar, se recoge una muestra y se evalúan diversos parámetros que influyen en la fertilidad. Esto es lo que mide un análisis de semen:
1. Volumen seminal
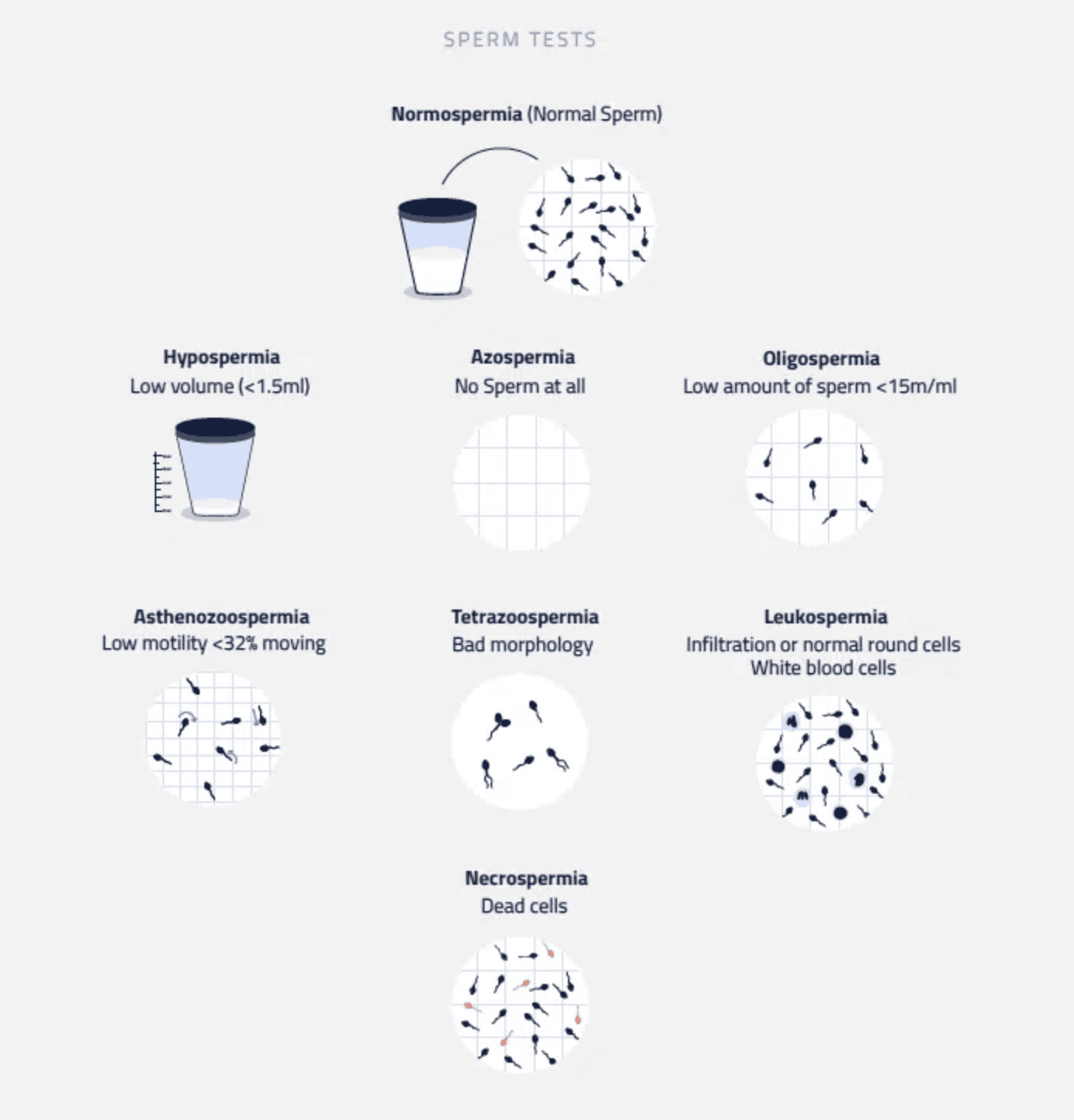
Se refiere a la cantidad total de líquido eyaculado. El volumen normal del semen oscila entre 2 y 5 mililitros (ml).
- Volumen bajo (<1,5 ml) (Hipospermia) → Posibles desequilibrios hormonales u obstrucciones
- Volumen elevado (>5,5 ml) (Hiperespermia) → Puede indicar una enfermedad subyacente
2. Recuento de espermatozoides (Concentración espermática)
El recuento de espermatozoides mide cuántos millones de espermatozoides hay por mililitro de semen.
- Normal: ≥15 millones de espermatozoides por mililitro
- Recuento de espermatozoides bajo (Oligospermia): <15 millones por ml
- Ausencia de espermatozoides (Azoospermia): Ausencia total de espermatozoides
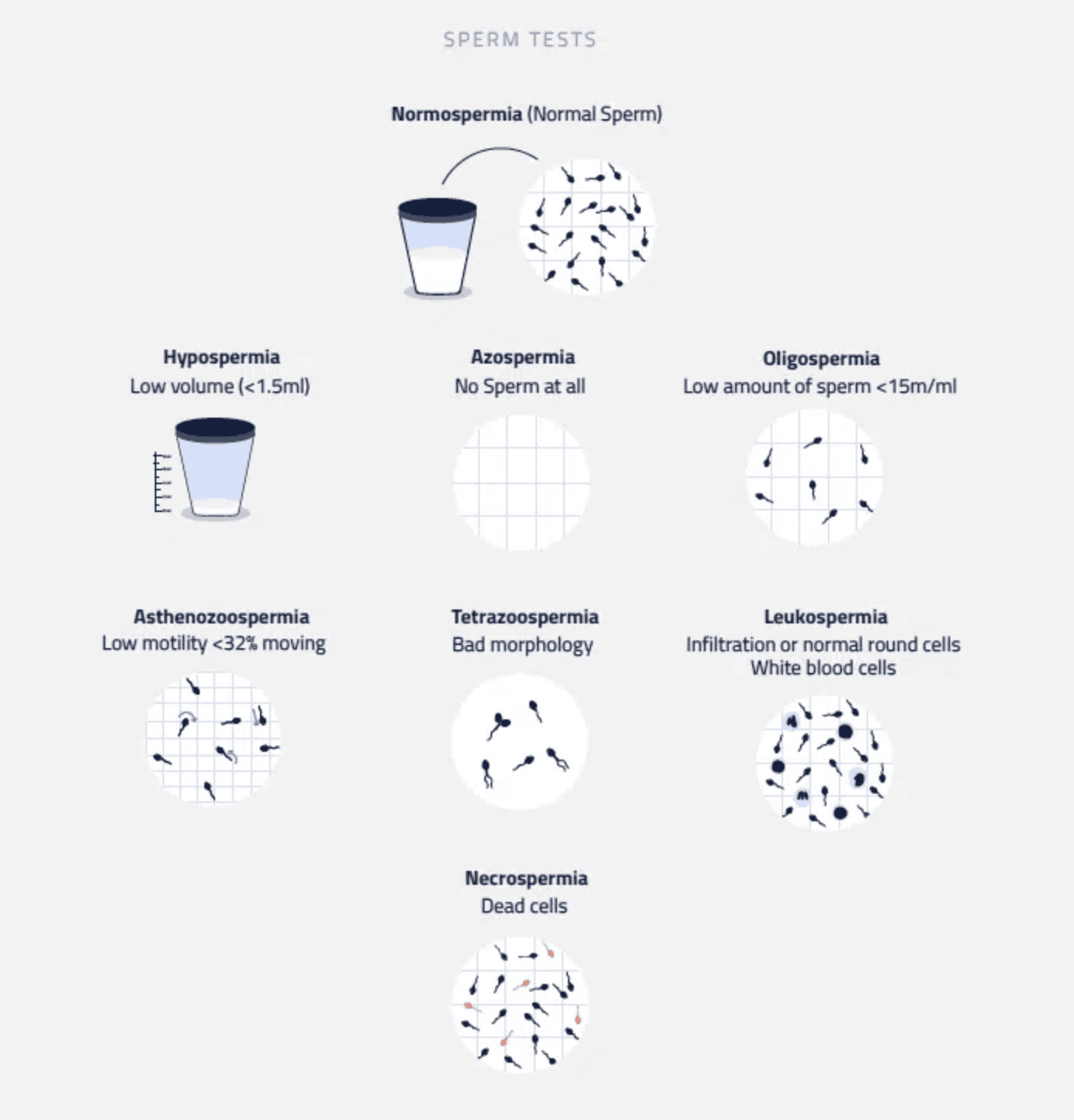
3. Motilidad espermática (capacidad de movimiento)
La motilidad de los espermatozoides determina lo bien que nadan hacia el óvulo. Se clasifica como:
- Motilidad Progresiva (MP): Los espermatozoides se mueven en línea recta o en grandes círculos
- Motilidad no progresiva (NP): Los espermatozoides muestran movimiento pero sin dirección efectiva
- Inmotilidad (MI): Ningún movimiento
Una muestra sana debe tener al menos un 32% de espermatozoides con motilidad progresiva, o un 40% si se incluye la motilidad no progresiva. Una motilidad deficiente, conocida como Astenozoospermia, puede reducir la probabilidad de concepción.
4. Recuento total de espermatozoides móviles (TMSC)
El TMSC representa el número total de espermatozoides móviles en el eyaculado, que se calcula multiplicando:
Volumen de semen (ml) × Concentración de espermatozoides (millones/ml) × Motilidad (%)
Un TMSC sano debe ser superior a 45 millones de espermatozoides para optimizar las posibilidades de fertilidad.
Parámetros adicionales del semen para un análisis más detallado
Si se detectan anomalías, puede ser necesario realizar un análisis de semen más avanzado, evaluando:
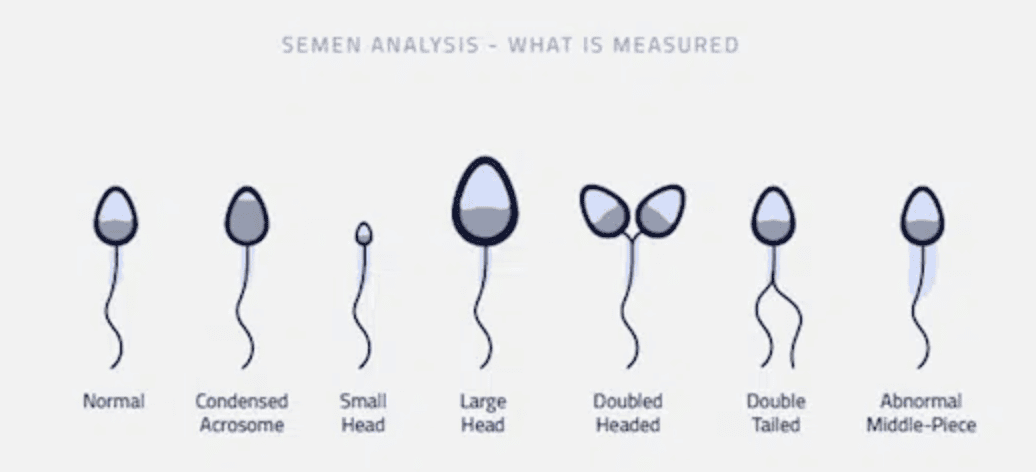
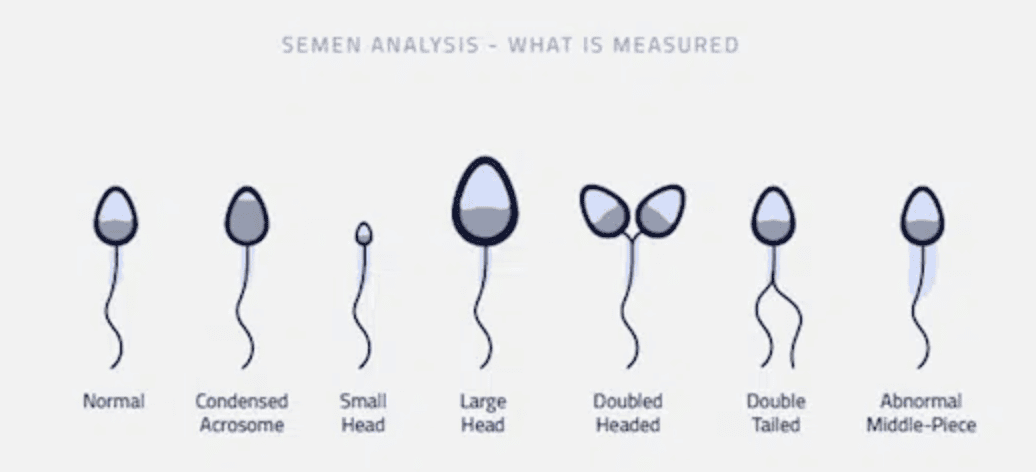
5. Morfología espermática (tamaño y forma)
La morfología espermática evalúa cuántos espermatozoides tienen una forma ovalada normal, según los estrictos criterios de Kruger:
Muestra normal: Al menos el 4% de los espermatozoides tienen una forma normal
Teratozoospermia: Menos del 4% de espermatozoides con forma normal
Los espermatozoides deformes pueden tener dificultades para moverse o penetrar en el óvulo, lo que afecta a la fertilidad.
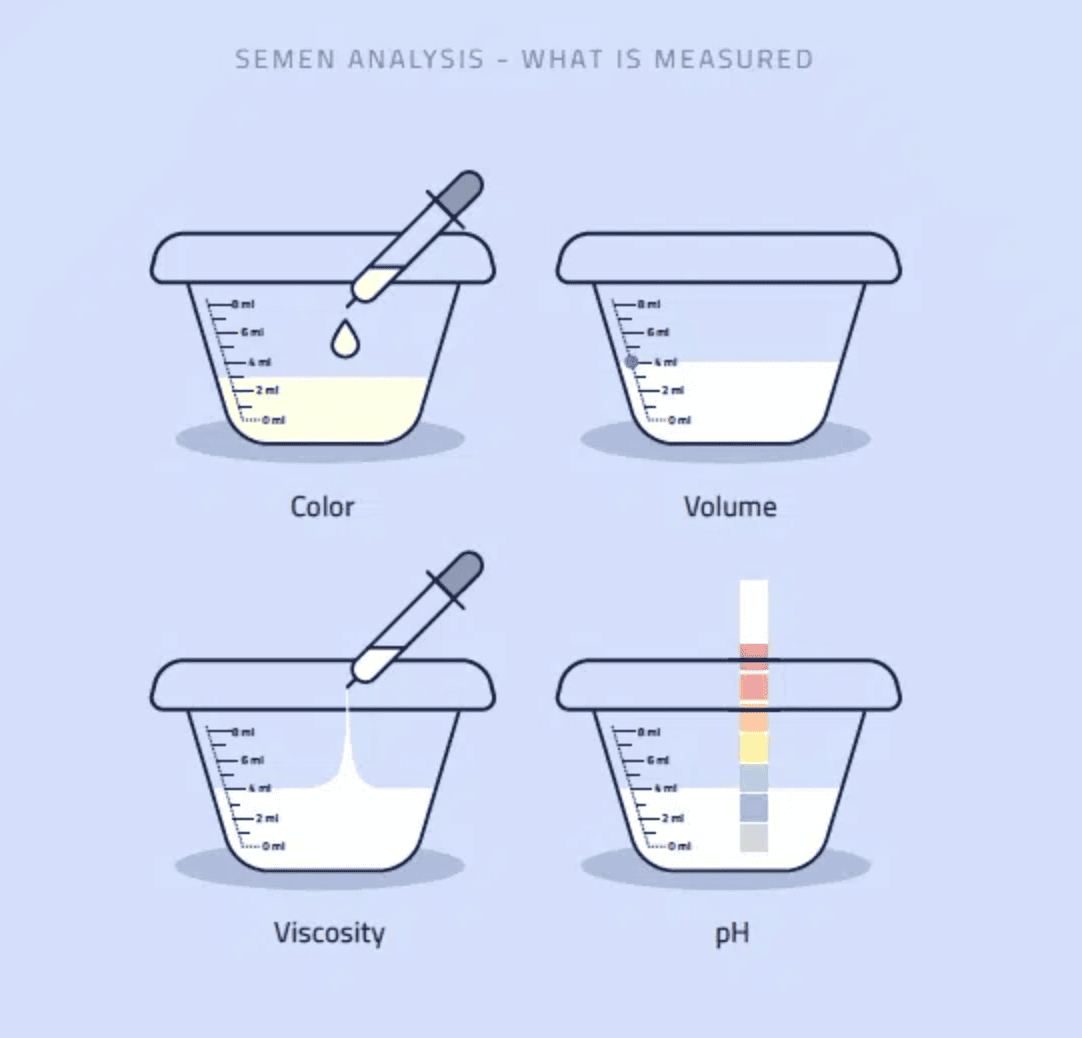
6. Color y viscosidad del semen
- Normal: Gris-opalescente
- Tinte rojo/marrón: Puede indicar sangre en el semen (Hemospermia)
- Viscosidad: El semen debe licuarse en 20 minutos; los retrasos pueden ser señal de infección.
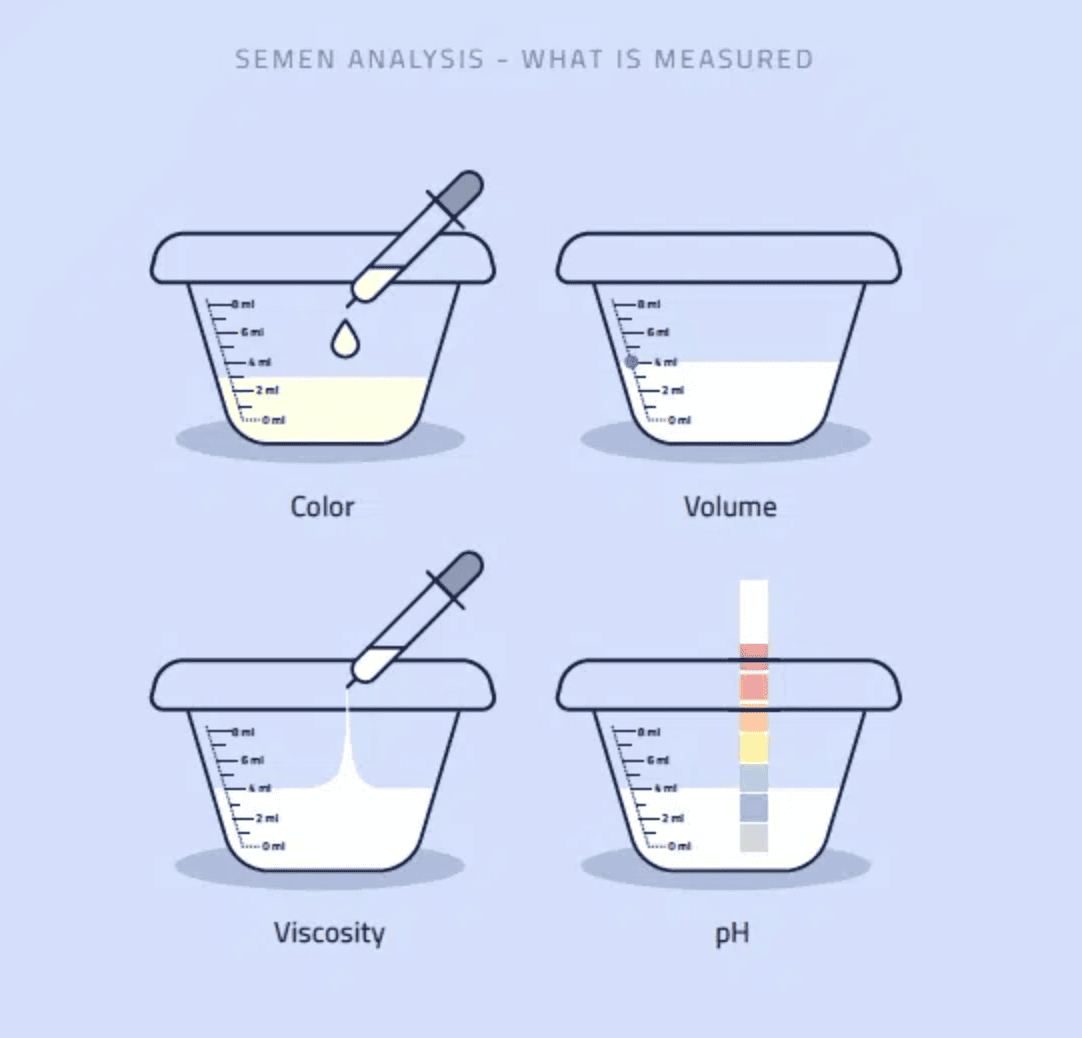
7. Niveles de pH del semen
El semen es ligeramente alcalino (pH 7,2-8,0). Los niveles anormales de pH pueden:
✔️ Matar los espermatozoides
✔️ Reducir la motilidad
✔️ Disminuir las posibilidades de fecundación
8. Vitalidad de los espermatozoides (espermatozoides vivos frente a muertos)
La vitalidad mide el porcentaje de espermatozoides vivos en una muestra. Un resultado normal es:
- ≥58% de espermatozoides vivos
- Necrozoospermia: Menos del 58% de espermatozoides viables
9. Glóbulos blancos (indicador de infección)
Unos glóbulos blancos elevados (leucospermia) pueden indicar infección o inflamación, lo que puede reducir la calidad del esperma.
10. Nutrientes esenciales en el semen
Ciertas sustancias del semen son cruciales para la función espermática:
- Zinc: ≥2,4 µmol/eyaculado
- Fructosa: ≥13 µmol/eyaculado (proporciona energía a los espermatozoides)
- Glucosidasa: ≥20 µU/eyaculado (relacionada con la maduración de los espermatozoides)
¿Por qué es importante un análisis de semen para la fertilidad masculina?
- Información rápida y fiable sobre la fertilidad
Un análisis de semen ofrece resultados rápidos que ayudan a detectar precozmente cualquier problema de fertilidad.
- Ayuda a mejorar la salud del esperma
Si los resultados son anormales, los ajustes en el estilo de vida (dieta, ejercicio, control del estrés) pueden mejorar la calidad del esperma en solo 72 días.
- Ahorra tiempo, dinero y tensión emocional
En lugar de meses (o años) de intentos infructuosos, un análisis precoz del semen ayuda a las parejas a tomar decisiones informadas cuanto antes.
- Indicador clave de la salud general
La mala calidad del semen puede ser un signo de desequilibrios hormonales, deficiencias nutricionales o incluso afecciones médicas subyacentes.