Download the Conceivio App
DownloadHow to Improve Your Chances of Pregnancy After Fertility Treatment

Mona Bungum
Article
8 min
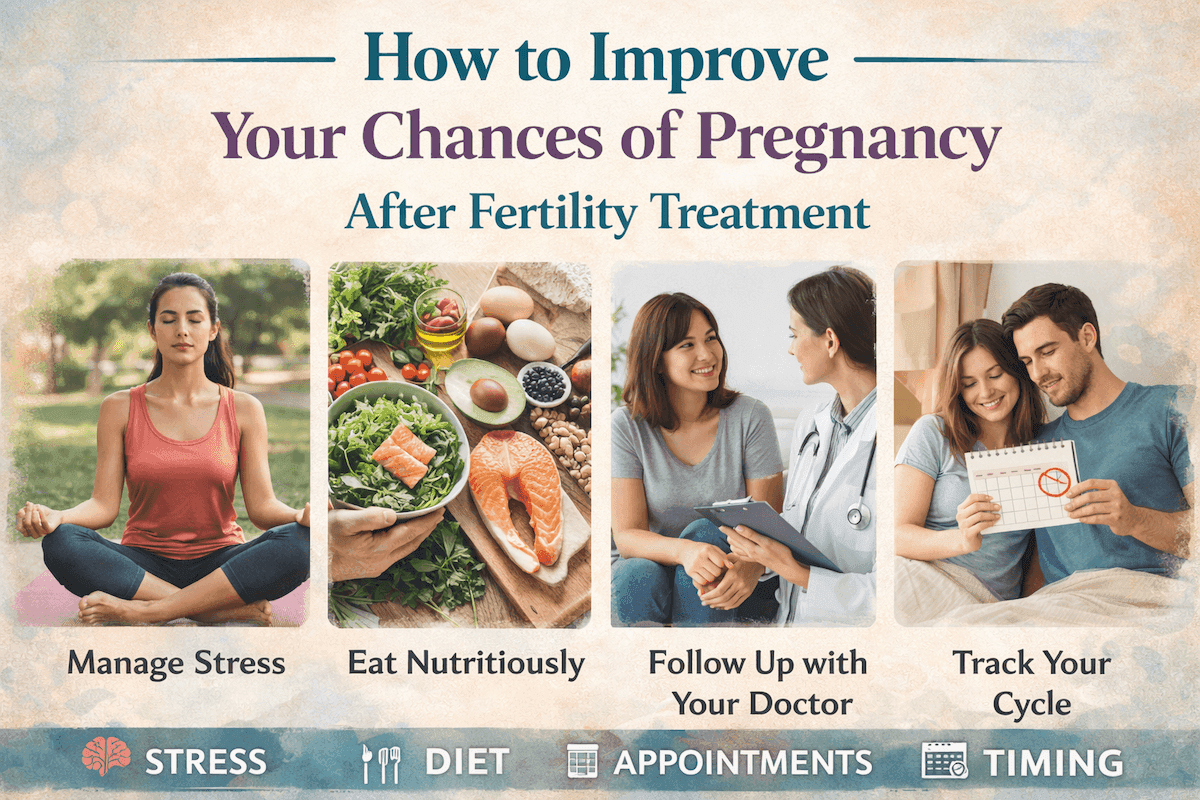
After fertility treatment, many people wonder what they can do themselves. This guide explains how lifestyle factors such as nutrition, sleep, stress, and metabolic health may support implantation and early pregnancy, without overstating what lifestyle can control.
When fertility treatment ends and an embryo is transferred or a stimulation cycle finishes, many women enter a quiet, uncertain waiting period. The medical steps are complete, but the outcome is still unknown. In this space, it is natural to look inward and wonder whether anything more can be done to support the process.
People often ask whether lifestyle choices can meaningfully influence what happens next, or whether everything is already out of their hands. The uncertainty can be heavy, especially when advice online ranges from rigid rules to dismissive reassurances that nothing matters.
Quick answer: There is no lifestyle change that can guarantee pregnancy or override embryo quality, genetics, or chance. However, evidence shows that habits affecting nutrition, sleep, movement, stress, and metabolic health can influence how the body responds after fertility treatment and may support healthier conditions for implantation and early pregnancy.
Fertility, Lifestyle, And The Body As A System
Fertility does not operate in isolation. Ovulation, implantation, and early pregnancy are influenced by a network of metabolic, hormonal, immune, and inflammatory processes that interact continuously.
Metabolic health affects hormone signalling. Inflammation influences egg quality and the uterine lining. Stress hormones interact with immune tolerance. Sleep regulates circadian rhythms that guide reproductive hormone release. When these systems are supported, the body may be better able to respond to fertility treatment and early pregnancy demands.
Lifestyle should be understood as a modifier rather than a determinant. People with excellent habits can still experience infertility, and others may conceive with fewer adjustments. What lifestyle offers is not control, but direction during a period that often feels passive.
Nutrition: Supporting Metabolic And Hormonal Balance
Nutrition influences fertility through insulin sensitivity, inflammatory signalling, oxidative stress, and energy availability, all of which interact with reproductive hormones and endometrial function.
Dietary patterns that emphasise vegetables, fruits, whole grains, legumes, lean proteins, and unsaturated fats are consistently associated with better reproductive outcomes. Mediterranean-style eating patterns have been linked with improved assisted reproduction results, partly because they support metabolic stability and reduce inflammatory load, a relationship also reflected in research on microplastics and fertility.
Large population studies show that diet quality matters more than isolated nutrients. Higher intake of ultra-processed foods has been associated with increased infertility risk, a pattern also seen in people later diagnosed with unexplained infertility.
For women managing hormonal conditions that affect insulin regulation, nutritional stability plays a particularly important role, which is why guidance on how to improve fertility with PCOS focuses on glucose balance rather than extreme dietary restriction.
What Practical Nutrition Support Looks Like
- Regular meals that avoid sharp blood sugar swings
- Whole foods prioritised over highly processed options
- A balance of vegetables, fruits, legumes, whole grains, and quality protein
- Healthy fats such as olive oil, nuts, seeds, and oily fish
Extreme diets, aggressive calorie restriction, or intermittent fasting immediately around embryo transfer are not supported by evidence and may increase physiological stress at a sensitive time.
Body Composition And Metabolic Health
Body weight alone does not determine fertility outcomes. What matters more is metabolic health, including how the body processes glucose, stores fat, and responds to insulin.
Excess abdominal fat is associated with chronic low-grade inflammation and insulin resistance, both of which can interfere with ovulation, egg quality, and endometrial receptivity. These mechanisms help explain why metabolic health matters without reducing fertility to a number on the scale.
Short-term weight loss efforts during treatment cycles have not been shown to reliably improve pregnancy rates and may increase stress. Evidence suggests that longer-term metabolic stability, supported by sustainable habits, is more relevant than rapid change.
For some women, underlying hormonal conditions such as PCOS can complicate metabolic regulation, which is why guidance around improving fertility with PCOS often focuses on insulin sensitivity rather than weight alone.
Physical Activity: Finding The Supportive Range
Movement supports insulin sensitivity, circulation, mood regulation, and sleep quality, all of which contribute to reproductive health.
Moderate activity such as walking, swimming, light cycling, or yoga is generally supportive before and after fertility treatment. These forms of movement improve metabolic function without placing excessive strain on the body.
Very intense or prolonged exercise without adequate energy intake can suppress reproductive hormones and disrupt ovulation. This effect is more likely when exercise becomes rigid or compulsive rather than supportive.
After embryo transfer, gentle activity helps maintain circulation and psychological wellbeing without increasing physical stress.
Sleep And Circadian Rhythms
Sleep plays a central role in hormone regulation, immune balance, and stress recovery. Disrupted or irregular sleep patterns can interfere with reproductive hormone signalling and are associated with menstrual irregularities and reduced fertility.
Consistent bedtimes, reduced evening screen exposure, and a dark, quiet sleeping environment help stabilise circadian rhythms. These rhythms influence cortisol, melatonin, and reproductive hormone release, all of which are active during early pregnancy.
Sleep disturbances are common during fertility treatment due to anxiety and hormonal changes. Addressing sleep gently rather than striving for perfection often leads to more sustainable improvement.
Stress: Separating Emotion From Physiology
Stress is one of the most misunderstood aspects of fertility. Emotional stress does not prevent implantation or cause treatment failure. Many people conceive during periods of intense emotional strain.
Chronic physiological stress, however, can influence fertility indirectly by disrupting sleep, increasing inflammation, and altering hormone balance. Stress dynamics often affect both partners, which helps explain why conversations around how men cope with fertility stress are relevant even when treatment is focused on the female body.
Predictable routines, social connection, and limiting exposure to overwhelming or contradictory fertility information often reduce physiological stress more effectively than attempts to suppress emotions. Understanding how men cope with fertility stress highlights that stress responses affect the body across genders and relationship dynamics.
Smoking, Alcohol, And Environmental Exposures
Certain exposures are consistently associated with reduced fertility and poorer treatment outcomes.
- Smoking affects egg quality, sperm DNA integrity, and uterine receptivity
- Alcohol, even at low levels, is best avoided around implantation and early pregnancy
- Caffeine intake up to around 200 mg per day is generally considered safe
Reasonable environmental precautions, such as reducing plastic food containers or avoiding unnecessary chemical exposure, can be part of a supportive lifestyle. Excessive vigilance, however, often increases anxiety without clear benefit.
Lifestyle And Fertility Before Treatment
Lifestyle patterns influence fertility long before treatment is required. Population studies show that women with healthier combined lifestyle behaviours, including diet quality, physical activity, waist circumference, smoking status, and alcohol intake, report significantly lower infertility rates.
These findings suggest that fertility reflects cumulative physiological conditions rather than isolated behaviours, a pattern also seen in people experiencing embryo development failure.
Avoiding The Trap Of Perfection
Lifestyle support is not about earning pregnancy through discipline. People conceive across a wide range of biological and behavioural contexts, and treatment outcomes are never a measure of effort or worth.
The evidence supports consistent, realistic habits that reduce physiological stress rather than rigid rules that generate anxiety. Focused routine matters more than constant monitoring.
FAQs About Lifestyle after Fertility Treatment
Can lifestyle changes really improve my chances of pregnancy after fertility treatment?
Lifestyle changes cannot override embryo quality, genetics, or chance, but they can influence how the body responds after treatment. Habits that support metabolic health, hormonal balance, sleep, and inflammation may help create more favourable conditions for implantation and early pregnancy.
What should I avoid doing after an embryo transfer?
There is no evidence that normal daily activities harm implantation. Extreme behaviours such as strict dieting, intense exercise, or constant symptom monitoring may increase physiological stress. Gentle routines and avoiding smoking and alcohol are more relevant than restriction or bed rest.
Does stress reduce my chances of pregnancy after IVF?
Emotional stress alone does not prevent pregnancy. However, chronic physiological stress can indirectly affect fertility by disrupting sleep, inflammation, and hormone regulation. Supporting routine, rest, and emotional safety is more helpful than trying to eliminate stress entirely.
Is diet important after fertility treatment is finished?
Yes, diet influences insulin sensitivity, inflammation, and energy availability, all of which play a role in early pregnancy physiology. A balanced, whole-food dietary pattern supports metabolic stability, while extreme dietary changes are not supported by evidence during this phase.
Should I exercise after embryo transfer?
Moderate physical activity such as walking or gentle yoga is generally safe and can support circulation and mental wellbeing. Very intense or prolonged exercise may place unnecessary stress on the body and is usually not recommended during the implantation window.
Does body weight affect pregnancy chances after fertility treatment?
Body weight alone does not determine outcomes. Metabolic health, including insulin sensitivity and inflammation, is more relevant. Short-term weight loss during treatment has not been shown to reliably improve pregnancy rates and may increase stress.
Can sleep really affect implantation and early pregnancy?
Sleep influences hormone regulation, immune balance, and stress recovery. Poor or irregular sleep may disrupt these systems. Consistent sleep routines support physiological conditions that are active during implantation and early pregnancy.
Should I take supplements to improve my chances after treatment?
There is no supplement that guarantees pregnancy. Supplements should only be used when recommended by a healthcare professional, based on individual needs. More is not better, and unnecessary supplementation can sometimes do more harm than good.
Does alcohol or caffeine matter after fertility treatment?
Alcohol is best avoided during the implantation window and early pregnancy. Moderate caffeine intake is generally considered safe, but excessive consumption may interfere with sleep and stress regulation, which indirectly affects reproductive physiology.
If this cycle fails, does it mean lifestyle changes didn’t work?
No. Fertility outcomes are influenced by many factors beyond lifestyle, including embryo genetics and chance. A negative outcome does not mean that lifestyle support was ineffective or that future cycles cannot succeed.
Where Support Can Make A Difference
Fertility and lifestyle science are often presented in fragmented or moralised ways, leaving many women unsure what truly matters. Evidence-based guidance helps distinguish supportive changes from unnecessary pressure.
At Conceivio, we provide inclusive fertility care grounded in science and compassion. Our resources are designed to help you make informed, calm decisions at every stage of your fertility journey.