Análisis de semen: Lo que la ciencia revela sobre la fertilidad masculina
La forma en que los médicos evalúan el esperma ha cambiado radicalmente. Lo que antes se limitaba a contar células al microscopio, ahora el moderno análisis de semen explora la integridad del ADN, el metabolismo energético y las señales moleculares que conforman la fertilidad. Lo que antes era un chequeo rutinario se ha convertido en una poderosa herramienta de diagnóstico que ofrece información sobre la salud reproductiva y general.
A pesar de estos avances, muchos hombres siguen dudando en someterse a una prueba de fertilidad masculina. La incomodidad social, el conocimiento limitado y las opiniones anticuadas siguen frenando las conversaciones sobre la salud del esperma. Sin embargo, comprender la ciencia que hay detrás de las pruebas puede ayudar a los hombres a tomar medidas informadas y seguras para mejorar la fertilidad y el bienestar a largo plazo.
Respuesta rápida: Un análisis de semen evalúa el recuento, la movilidad, la forma y la calidad del ADN de los espermatozoides para determinar el potencial de fertilidad. Las pruebas modernas pueden detectar problemas sutiles relacionados con el estilo de vida, las hormonas o el estrés oxidativo. Estos conocimientos ayudan a diagnosticar precozmente la infertilidad masculina y orientan los planes personalizados para mejorar la calidad del esperma y la salud general.
Por qué el análisis de semen es más importante que nunca
Un análisis de semen estándar proporciona tres medidas clave: conteo, motilidad y morfología. Estas siguen siendo la base de las pruebas de fertilidad masculina, pero los investigadores comprenden ahora que sólo revelan una parte de la historia.
Los espermatozoides sanos hacen algo más que nadar eficientemente. Cada uno transporta material genético, reservas de energía y "mensajes" moleculares que influyen en la concepción y el desarrollo embrionario. La evaluación de estas capas de información permite a los médicos identificar problemas que un microscopio tradicional podría pasar por alto.
Por ejemplo, un daño sutil en el ADN de los espermatozoides puede afectar al éxito de la fecundación aunque los recuentos parezcan normales. La detección precoz de estos problemas mediante un análisis de semen ayuda a los médicos a recomendar tratamientos específicos o cambios en el estilo de vida para mejorar la función espermática y los resultados reproductivos.
Un vistazo más de cerca al proceso de análisis
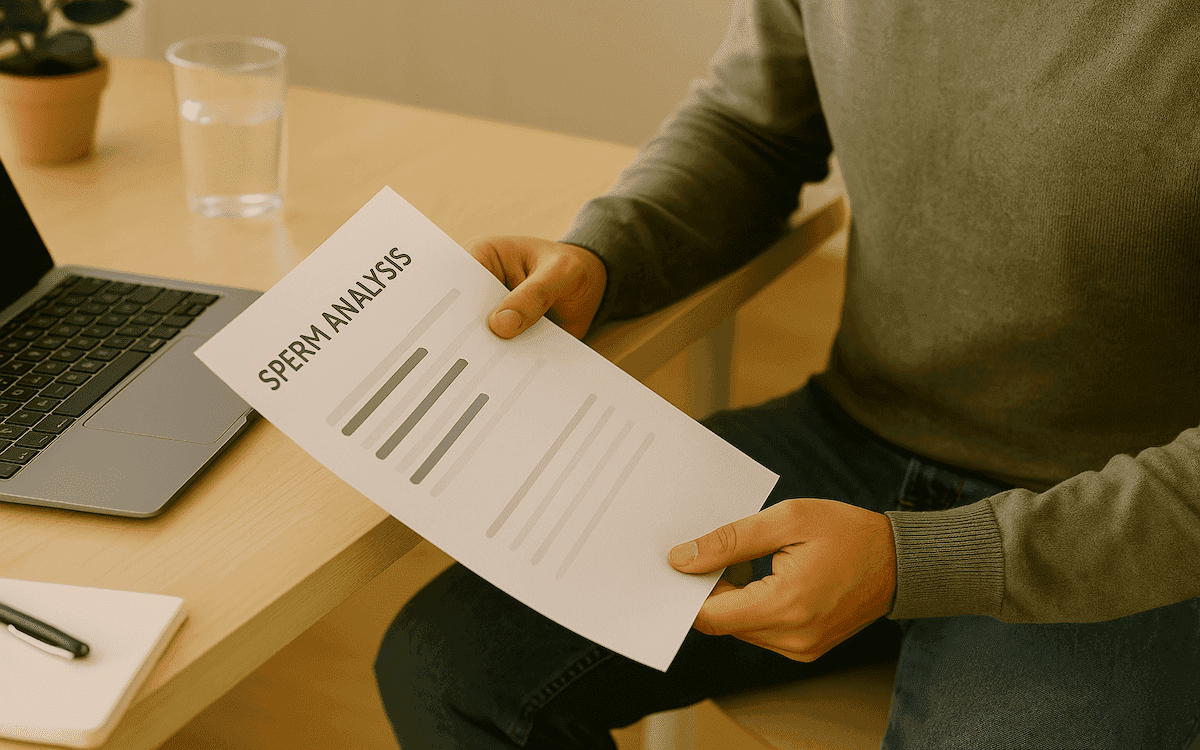
Durante un análisis de semen, se recoge una muestra de semen y se examina en un laboratorio de fertilidad. Los técnicos evalúan el número de espermatozoides, lo bien que se mueven y si sus formas se ajustan a parámetros saludables.
Los laboratorios modernos también realizan evaluaciones avanzadas, como:
- Análisis de fragmentación del ADN, que identifica daños genéticos que pueden reducir la calidad embrionaria.
- Pruebas de estrés oxidativo, que miden los desequilibrios que dañan las membranas y el ADN de los espermatozoides.
- Pruebas de estructura de la cromatina, que evalúan la densidad del ADN en el interior de la cabeza del espermatozoide.
- Análisis con inteligencia artificial (IA), que identifican automáticamente los espermatozoides más sanos para su uso en reproducción asistida.
Estas innovaciones proporcionan una imagen completa de la fertilidad masculina, orientando los tratamientos que se dirigen tanto a las causas biológicas como a las relacionadas con el estilo de vida.
Del recuento de células a la comprensión de la biología
El análisis tradicional del semen trataba los espermatozoides como números en un informe. Hoy en día, los científicos comprenden que la fertilidad depende de algo más que de la cantidad. La capacidad de un espermatozoide para moverse, penetrar en el óvulo y entregar ADN intacto es fundamental para el éxito de la concepción.
Los estudios han revelado que la salud de los espermatozoides depende en gran medida del metabolismo energético, la capacidad de las mitocondrias de generar suficiente energía para el largo viaje hasta el óvulo. Cuando los sistemas energéticos fallan, los espermatozoides pierden movilidad y función.
Una prueba de fertilidad masculina que incluya marcadores de energía y estrés oxidativo puede identificar estos puntos débiles antes de que provoquen infertilidad. Comprender cómo funcionan estos procesos biológicos permite a los médicos personalizar el tratamiento, desde los antioxidantes hasta la gestión hormonal y la nutrición específica.
Integridad del ADN y pruebas genéticas
La calidad del ADN de un hombre influye directamente en los resultados de la fertilidad. Aunque el recuento y el movimiento de los espermatozoides parezcan normales, una fragmentación elevada del ADN puede reducir las posibilidades de embarazo o aumentar el riesgo de aborto.
Los laboratorios modernos incluyen ahora el análisis de fragmentación del ADN como parte de las pruebas espermáticas avanzadas. Esta evaluación busca roturas en los filamentos genéticos, a menudo causadas por el estrés oxidativo, el tabaquismo, una dieta deficiente o la exposición a toxinas ambientales.
Al identificar precozmente el ADN dañado, las parejas pueden evitar retrasos innecesarios y seguir opciones de tratamiento con mejores tasas de éxito. Aprender qué significa la fragmentación del ADN espermático puede ayudar a los hombres a comprender por qué un ADN sano es tan importante como el recuento o la motilidad.
El papel del estilo de vida y el entorno
Los hábitos cotidianos tienen un impacto mensurable en la salud del esperma. Las investigaciones demuestran sistemáticamente que la nutrición, los niveles de estrés y la exposición ambiental influyen en la calidad del esperma.
Los alimentos ricos en antioxidantes, la actividad física regular y un sueño adecuado pueden mejorar significativamente la motilidad del esperma y reducir los daños en el ADN. Por el contrario, el estrés elevado, el tabaquismo, el consumo de alcohol y la falta de ejercicio pueden reducir la calidad y el recuento de espermatozoides.
Una sencilla prueba de recuento espermático puede revelar cómo influyen las elecciones de estilo de vida en la fertilidad. Hacer pequeñas mejoras constantes, como añadir ácidos grasos omega-3, reducir los alimentos procesados y mantener un peso corporal saludable, puede revertir muchos problemas de fertilidad temprana. Para obtener orientación sobre cambios positivos, explora cómo mejorar la salud del esperma mediante pasos prácticos.
Las toxinas ambientales también influyen. Las sustancias químicas de los plásticos, la contaminación atmosférica y los pesticidas se han relacionado con una menor calidad del esperma. Los hombres que trabajan en entornos industriales o de alta exposición deben considerar la posibilidad de someterse a pruebas periódicas de fertilidad para controlar los posibles efectos a lo largo del tiempo.
El lado emocional de las pruebas de fertilidad masculina
Los problemas de fertilidad no son sólo biológicos, sino también emocionales. A muchos hombres les cuesta hablar de las pruebas de esperma por miedo, vergüenza o ideas erróneas sobre la masculinidad.
Reconocer estos sentimientos es esencial. Una prueba de infertilidad masculina no mide la autoestima ni la masculinidad; mide la biología. Proporciona respuestas que capacitan a los hombres y a las parejas para avanzar con claridad y no con conjeturas.
Hablar abiertamente de los resultados también puede reforzar la comunicación entre los miembros de la pareja. Compartir el proceso fomenta la comprensión mutua y reduce la culpa o el sentimiento de culpabilidad. En Conceivio, animamos a los hombres a ver las pruebas de fertilidad como un acto de autoconocimiento, no de vergüenza.
La ciencia del estrés oxidativo
El estrés oxidativo se produce cuando las moléculas dañinas conocidas como radicales libres superan en número a los antioxidantes naturales del organismo. Este desequilibrio daña las membranas y el ADN del esperma, reduciendo la motilidad y la calidad general.
Los investigadores han descubierto que el estrés oxidativo es uno de los factores que más contribuyen a la infertilidad masculina. Afortunadamente, también es uno de los más tratables. La terapia antioxidante, la reducción del estrés y los ajustes del estilo de vida pueden restablecer el equilibrio y mejorar los resultados de la fertilidad.
Aprender sobre las conexiones entre testosterona, estrés y fertilidad masculina ayuda a los hombres a reconocer cómo influyen la salud emocional y física en el éxito reproductivo.
La tecnología y el futuro de las pruebas de fertilidad
La evolución de la ciencia de la fertilidad está remodelando la forma en que las clínicas abordan el diagnóstico y el tratamiento. La inteligencia artificial desempeña ahora un papel central en la evaluación del esperma. Los microscopios impulsados por IA pueden analizar miles de espermatozoides en segundos, detectando patrones que predicen el éxito de la fecundación.
Esta tecnología es especialmente útil para procedimientos como la ICSI (inyección intracitoplasmática de espermatozoides), en la que los embriólogos seleccionan espermatozoides individuales para la fecundación. Al automatizar este proceso, la IA mejora la precisión y aumenta la probabilidad de resultados positivos.
Los investigadores también están explorando cómo la ciencia de las células madre podría ayudar a los hombres que no tienen esperma viable debido a afecciones genéticas o médicas. Los primeros experimentos sugieren que el esperma podría desarrollarse a partir de células madre o tejido testicular conservado, dando nuevas esperanzas a parejas que antes no tenían opciones.
La salud del esperma como reflejo del bienestar general
La salud del esperma suele ser un espejo del bienestar más general. Los hombres con mejores parámetros espermáticos tienden a vivir más tiempo y a sufrir menos enfermedades crónicas. Esto se debe a que los mismos sistemas biológicos que regulan las hormonas de la fertilidad, el metabolismo y el equilibrio oxidativo también influyen en la salud cardiovascular y metabólica.
En este sentido, un análisis de esperma es más que una herramienta de fertilidad; es un indicador precoz de la salud sistémica. Los análisis regulares animan a los hombres a controlar los cambios a lo largo del tiempo y a tomar decisiones preventivas sobre su estilo de vida. Comprender cómo afecta la edad a la fertilidad masculina también puede ayudar a planificar con antelación el bienestar reproductivo a largo plazo.
El enfoque holístico de la fertilidad masculina
La atención moderna a la fertilidad se centra ahora en la persona en su totalidad. En lugar de tratar los resultados aislados de las pruebas, las clínicas evalúan los factores biológicos, psicológicos y de estilo de vida que conforman la salud reproductiva.
Un análisis completo de fertilidad masculina puede incluir análisis hormonales, pruebas de estrés oxidativo, evaluaciones nutricionales y revisiones del estilo de vida. Así, los planes de tratamiento personalizados pueden abordar las causas profundas y no sólo los síntomas.
En Conceivio, nuestro enfoque combina la ciencia con la empatía. Ayudamos a los hombres a comprender los datos que hay detrás de sus resultados y les proporcionamos medidas prácticas para mejorar. Tanto si implica tratamiento médico, asesoramiento o apoyo nutricional, la atención holística ayuda a las parejas a abordar la fertilidad como un viaje compartido.
Preguntas frecuentes sobre el análisis de semen
1. ¿Cuál es la precisión de un análisis de semen?
Cuando lo realizan laboratorios acreditados, el análisis de semen es muy fiable para evaluar el recuento, la motilidad y la morfología de los espermatozoides. Sin embargo, los resultados pueden variar entre muestras, por lo que los médicos suelen recomendar dos o más pruebas tomadas con algunas semanas de diferencia.
2. ¿Pueden los cambios en el estilo de vida mejorar los resultados del análisis de semen?
Sí. Hacer ejercicio con regularidad, llevar una alimentación equilibrada, reducir el estrés y evitar fumar o beber alcohol en exceso pueden mejorar notablemente la calidad del esperma en pocos meses.
3. ¿Qué se considera un recuento espermático normal?
Según la Organización Mundial de la Salud, un recuento espermático saludable es de unos 15 millones de espermatozoides o más por mililitro de semen. Un número inferior no siempre significa infertilidad, pero puede reducir la probabilidad de concepción natural.
4. ¿Por qué un análisis de semen puede dar resultados normales y aun así no producirse el embarazo?
Los análisis de semen estándar no pueden detectar problemas moleculares más profundos, como la fragmentación del ADN espermático o el estrés oxidativo. En estos casos, los médicos pueden sugerir pruebas adicionales para examinar la calidad genética y celular del esperma.
5. ¿Con qué frecuencia deben los hombres repetir un análisis de semen?
Si los resultados son anormales, suele recomendarse repetir la prueba al cabo de dos o tres meses, el tiempo que tardan en desarrollarse nuevos espermatozoides. Los hombres que intentan activamente concebir o que siguen un tratamiento pueden repetir la prueba cada pocos meses para controlar los progresos.
Dar el primer paso
Un análisis de semen es sencillo, discreto y muy informativo. Proporciona a los hombres claridad sobre su potencial de fertilidad y sienta las bases para una atención personalizada.
Ignorar los problemas de fertilidad sólo retrasa las respuestas. Si se hacen las pruebas pronto, los hombres pueden descubrir problemas corregibles y evitar tensiones emocionales y económicas innecesarias. Un solo análisis de semen puede marcar la diferencia entre la incertidumbre y el empoderamiento.