The Vaginal Microbiome: A Key Factor in Predicting IVF Success

Aisling Fourie
Article
4 min
This article explores how an imbalance in the vaginal microbiome, especially a lack of Lactobacillus, can affect fertility and lower IVF success rates. It discusses how vaginal infections like bacterial vaginosis and yeast overgrowth can impact reproduction, and how testing and treatment can help improve outcomes.
The journey through in vitro fertilisation (IVF) is often complex and emotionally charged. Many factors from hormone balance to egg and sperm quality influence outcomes. Increasingly, researchers are also examining a lesser-known piece of the fertility puzzle: the vaginal microbiome.
Early studies indicate that the microorganisms living in the vagina might play a role in reproductive health, possibly influencing implantation and early pregnancy. However, while the findings are intriguing, the science is still developing, and results are not yet consistent across studies.
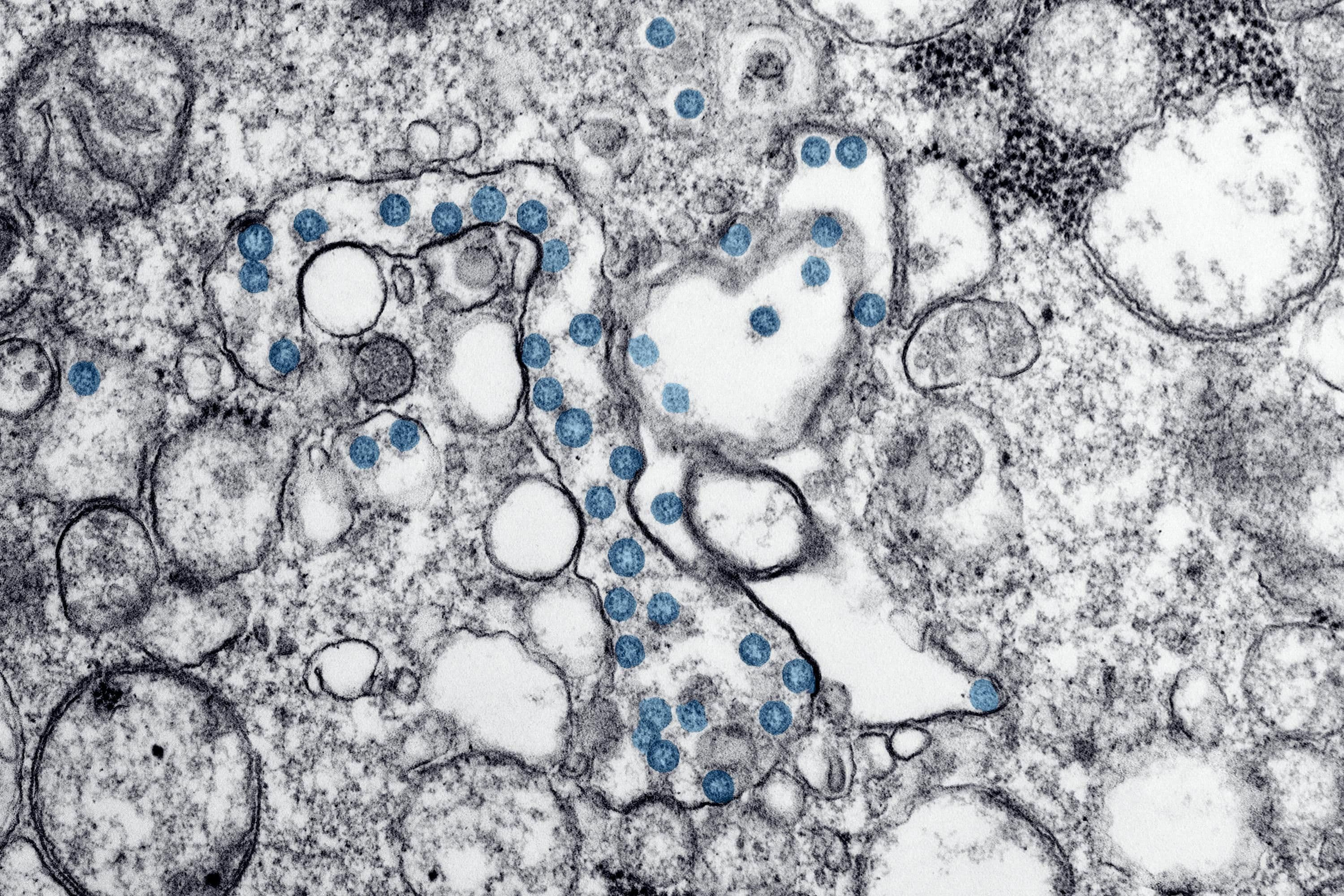
1. What is the vaginal microbiome, and why might it matter for fertility?
The vaginal microbiome is a community of bacteria, fungi, and viruses that live in the vaginal canal. Unlike the gut, which benefits from diversity, the vaginal microbiome appears healthiest when dominated by Lactobacillus species. These bacteria help maintain a low pH (around 4.5), which discourages harmful microbes and supports a balanced environment.
When this balance shifts a condition known as dysbiosis inflammation can increase, potentially affecting cervical mucus, sperm survival, and implantation conditions.
Links to IVF outcomes
Some small studies, such as one published in the National Library of Medicine, have observed that women with Lactobacillus-dominant microbiomes tend to have better implantation and live birth rates compared to those with microbial imbalances like Gardnerella vaginalis or Atopobium vaginae.
Still, researchers caution that these associations don’t prove causation and larger, controlled studies are needed to confirm whether the vaginal microbiome can reliably predict IVF outcomes.
2. Inflammation and its potential role in IVF and pregnancy
The inflammation–fertility connection
Inflammation is a normal immune response, but when it becomes chronic, it can interfere with conception. Some evidence suggests that inflammatory markers in the uterus or vagina, such as cytokines IL-6 and TNF-alpha, may be linked to implantation failure or early miscarriage (Frontiers in Immunology).
However, it’s unclear whether inflammation directly causes these outcomes or simply reflects other underlying issues like infection or hormonal imbalance.
During pregnancy
Ongoing low-grade inflammation has been associated with complications like preterm birth, preeclampsia, and pregnancy loss (PubMed, 2022). Managing inflammation through balanced nutrition and microbiome support may help, though clinical proof remains limited.
3. Lifestyle factors that might influence the vaginal microbiome
The vaginal microbiome responds to diet, stress, and lifestyle habits — all of which are especially relevant during fertility treatment.
Alcohol and fertility
Even moderate alcohol intake can influence hormone balance and inflammation. A study on IVF outcomes found that women consuming more than four drinks per week had a lower chance of conception. Reducing or avoiding alcohol at least a few months before IVF may support hormone stability and overall reproductive health.
4. Hormones, microbiome, and egg quality: a possible connection
How hormones shape vaginal bacteria
Oestrogen promotes glycogen production in vaginal cells, providing food for Lactobacillus, while progesterone influences immune and mucus function. When hormone levels fluctuate due to stress, medication, or diet the microbiome can shift, potentially raising inflammation risk.
Nutrition and egg quality
Systemic inflammation can also affect egg health. Diets rich in omega-3 fatty acids, antioxidants, and micronutrients like CoQ10, zinc, and vitamins C and E may help protect eggs from oxidative damage. Though evidence is preliminary, supporting overall metabolic and inflammatory health is widely seen as beneficial during IVF preparation.
5. Can you test and improve your vaginal microbiome before IVF?
Testing options
Vaginal microbiome testing can identify bacterial balance using a simple swab. Clinics and at-home kits can detect common imbalances involving Gardnerella, Ureaplasma, or Candida species.
When dysbiosis is found, approaches may include:
- Probiotics (especially Lactobacillus crispatus)
- Dietary improvements with fibre and fermented foods
- Stress and sleep management
- Medical treatment, when infection is present
Though some clinics offer microbiome testing as part of pre-IVF assessments, experts note that the field is still in its early stages, and standardized treatment guidelines are lacking.
6. Supporting vaginal and reproductive health naturally
To maintain a balanced microbiome and stable hormone levels:
- Follow a Mediterranean-style diet rich in fibre, healthy fats, and antioxidants
- Avoid excessive sugar, processed foods, and alcohol
- Maintain a healthy weight and regular exercise
- Refrain from using douches or scented products
- Prioritize sleep and stress management
These steps can help reduce inflammation and support overall fertility, even beyond microbiome effects.
7. AMH levels, inflammation, and fertility potential
Anti-Müllerian hormone (AMH) reflects ovarian reserve and may also be influenced by overall metabolic health. While there’s no proven way to significantly increase AMH, optimising nutrition and lowering inflammation can support ovarian function.
Key steps include:
- Ensuring adequate vitamin D, omega-3s, and CoQ10
- Limiting alcohol and sugar intake
- Eating protein-rich foods and anti-inflammatory ingredients like turmeric and olive oil
8. Can lifestyle improve egg quality? Possibly.
Although age remains the strongest determinant of egg quality, research suggests that nutrition, inflammation control, and antioxidant intake may improve fertilisation potential. For example, anti-inflammatory dietary patterns have been linked to better embryo development in women undergoing IVF (Reproductive Medicine).
9. The vaginal microbiome: a promising but unproven predictor
A 2023 meta-analysis suggested that vaginal microbial composition might correlate with IVF success, but the evidence is still preliminary. While microbiome assessment could one day become part of standard fertility screening, it’s currently best viewed as an emerging research tool rather than a proven predictor.
Final thoughts: nurturing balance for better fertility
Your vaginal microbiome is an active part of your reproductive system one that interacts with hormones, immunity, and inflammation. Although more studies are needed, supporting microbial balance through healthy habits, good nutrition, and inflammation management can help create the best possible foundation for conception and pregnancy.