Fertility and Stress: How Deep Breathing Help Restore Hormonal Balance

Mona Bungum
Article
8 min
Discover how stress affects fertility and how deep breathing for stress relief can lower cortisol, regulate hormones, and support your journey to conception.
Stress and fertility are deeply connected, yet most people only discover this once they’re already struggling to conceive. Hormones don’t operate in isolation. They respond to your environment, your thoughts, your routines, and even the rhythm of your breath. When stress rises and stays high, the body quietly shifts into protection mode and reproduction is one of the first systems to slow down.
For many women, this connection becomes clear only after months or years of trying. That was the case for Emma, whose fertility journey began with optimism but slowly became overshadowed by pressure, tension, and intrusive worry. What she didn’t realize at the time was how tightly her nervous system was gripping every part of her reproductive health.
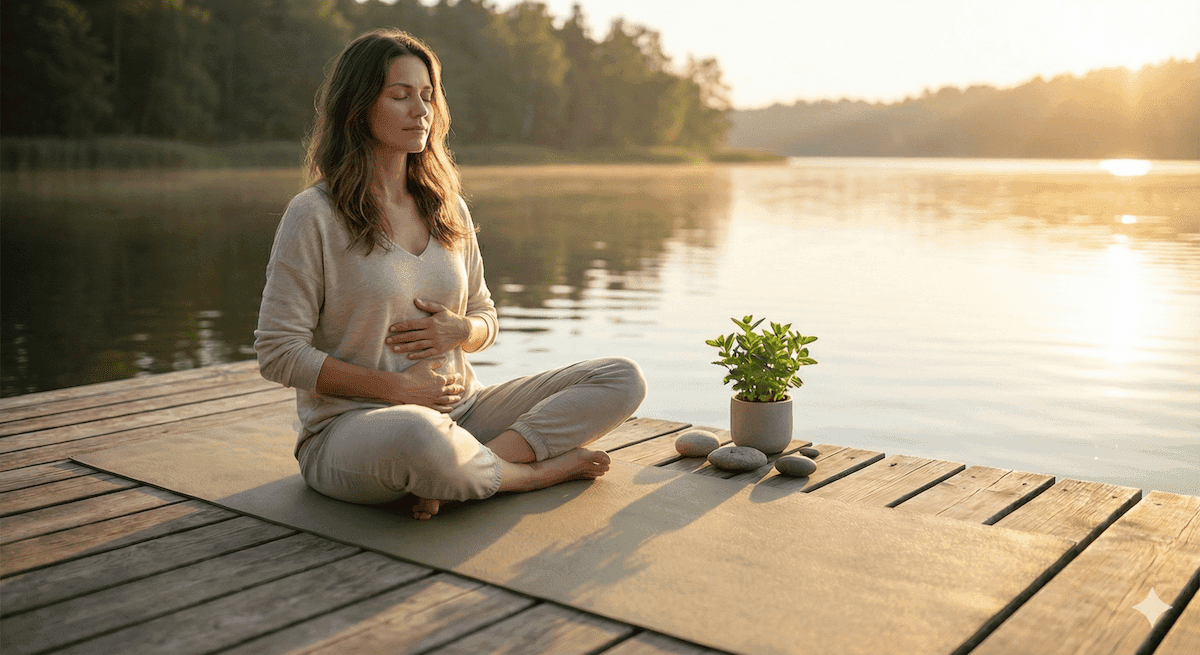
Her turning point arrived not through medication or a new test result, but through a conversation that reframed everything: your body can only ovulate when it feels safe. The simplest tool that helped her reconnect safety with her physiology wasn’t expensive or complicated it was deep breathing, used consistently as a form of nervous system repair. This article explores how fertility and stress interact, why breathing matters, and how small daily practices can gradually shift your hormonal landscape back into balance.
Why Stress Disrupts Fertility: The Physiology You Can’t Ignore
Stress is not an emotional weakness, it’s a hormonal cascade. When your brain senses uncertainty, overwhelm, or fear, it activates the HPA axis (hypothalamic–pituitary–adrenal system). Cortisol increases, heart rate rises, blood sugar spikes, and energy is diverted to survival processes.
Reproduction requires calm, stability, and hormonal synchrony. Chronic stress disrupts each of these.
The domino effect of stress on the reproductive system
1. Suppressed ovulation
Elevated cortisol interferes with LH and FSH, the hormones that grow follicles and trigger egg release. Research shows that sustained stress can delay or even prevent ovulation altogether. This is explored further in Conceivio’s guide on the biological connection between stress and fertility which helps explain why cycles become irregular when stress peaks.
2. Impaired progesterone balance
Stress pushes the body toward cortisol production and away from progesterone synthesis. Low progesterone can shorten the luteal phase, affect implantation, or contribute to early losses.
3. Reduced sexual desire
High cortisol naturally drives down libido, not due to lack of interest, but to protect the body from conception during danger.
4. Inflammation and oxidative stress
Chronic tension increases inflammatory molecules that impair egg quality and affect uterine receptivity.
And importantly, stress affects men’s fertility too. Studies show cortisol disrupts testosterone production, increases oxidative stress in testicular tissue, and worsens sperm DNA integrity. Conceivio explores this in more detail in the research-based guide on testosterone, stress, and male fertility a reminder that fertility is always a two-person physiology.
Emma’s Story: From Shallow Breaths to a Calmer Body
When Emma and her partner began trying, she did everything “right.”
She tracked ovulation, optimized food choices, drank more water, exercised gently, and reduced caffeine. But emotionally she felt increasingly brittle. She woke up with tight shoulders, clenched her jaw without noticing, and switched between hope and fear every month. Her breathing was so shallow that she sometimes felt lightheaded in the afternoon.
One day her fertility specialist said, kindly:
“Your body can’t ovulate well when it’s bracing.”
Those words lingered with Emma for days. She realized she had been living in a cycle of vigilance constantly checking apps, interpreting symptoms, reading forums, and anticipating disappointment. Her nervous system was signaling danger, not safety.
She enrolled in a mind-body program that introduced her to deep breathing techniques. At first it felt too simple to be effective, but within a week she noticed:
- Her heart rate settling
- Fewer afternoon headaches
- Easier sleep onset
- Less fixation on cycle tracking
Within a couple of months, her cycles stabilized, PMS reduced, and she described feeling “more present in my body than I have in years.”
Breathing didn’t fix everything but it unlocked the calm she needed for her physiology to work again.
How Deep Breathing Rebalances Stress and Fertility
Deep breathing is one of the fastest ways to shift your body out of stress mode and into hormonal safety. This isn’t spiritual or symbolic, it’s neuroendocrine science.
1. Activation of the vagus nerve
Slow breathing stimulates the vagus nerve, shifting the nervous system into its parasympathetic state (“rest and digest”). This directly lowers cortisol and helps restore reproductive signaling.
2. Improved oxygenation of reproductive tissues
Deep inhalations improve circulation to the ovaries, uterus, and abdominal organs, enhancing nutrient delivery.
3. Reduced muscle tension around the pelvis
Chronic stress tightens abdominal and pelvic muscles, which may negatively influence menstrual comfort and blood flow.
4. Better hormone regulation
Breathing affects heart rate variability (HRV), a measure strongly linked to hormonal balance and resilience.
5. Emotional grounding
Deep breathing for stress relief helps reduce spiraling thoughts that fuel anxiety and keeps the fertility journey from becoming emotionally overwhelming.
Breathing Techniques That Help Reset Your Nervous System
Fertility does not require perfection, it requires consistency. These techniques can be used throughout the day, and each one encourages both emotional calm and hormonal stability.
Diaphragmatic Breathing (Emma’s daily staple)
This is the foundation of all restorative breathwork.
- Sit or lie down comfortably.
- Place one hand on your chest and one on your belly.
- Inhale slowly through your nose, expanding your abdomen.
- Exhale fully, letting your belly fall.
- Continue for 5–10 minutes.
A 2020 clinical trial showed that daily diaphragmatic breathing significantly reduces cortisol and improves anxiety outcomes in women under fertility-related stress.
Box Breathing for moments of panic
Useful before blood tests, appointments, or pregnancy test days.
- Inhale 4 seconds
- Hold 4 seconds
- Exhale 4 seconds
- Hold 4 seconds
- Repeat 4–6 times
This technique is commonly used by athletes to regulate focus under pressure.
Alternate Nostril Breathing (for emotional balance)
A powerful practice for mood stability and reducing internal agitation.
- Close right nostril, inhale left
- Switch, exhale right
- Inhale right
- Switch, exhale left
- Continue 3–5 minutes
A 2022 review found this method helpful for regulating cortisol and improving emotional clarity.
Breathing Isn’t Enough Alone, You Need Daily Nervous System Support
Breathwork works best when combined with supportive habits that keep your body out of chronic stress loops.
1. Sleep deeply and consistently
Your cycle hormones regulate during sleep, especially melatonin and progesterone. Poor sleep disrupts cycle timing and ovulation. Conceivio’s guide on sleep and fertility explains how disrupted rest interferes with reproductive signaling and why sleep must be treated as hormone care, not luxury.
2. Address ongoing stress patterns
Some stressors can be reduced; others need to be managed. Conceivio’s insights on managing stress provide practical, evidence-backed strategies that complement breathing and support long-term hormonal recovery.
3. Identify emotional triggers early
Many women experience stress spikes around ovulation, the two-week wait, or after negative tests. Conceivio’s guide on how men cope with fertility-related stress offers insights that apply across partners and highlights the emotional patterns that often appear during TTC journeys.
These steps, paired with breathwork, help create a more stable internal environment, the foundation for healthy ovulation, implantation, and long-term reproductive wellbeing.
FAQs About Fertility and Stress
Can stress really affect fertility?
Yes. Chronic stress raises cortisol, which disrupts the hormones responsible for ovulation, implantation, and menstrual cycle regularity. When stress stays high for long periods, the reproductive system slows down because the body prioritizes survival over conception.
Does stress delay ovulation?
It can. Elevated cortisol interferes with FSH and LH, the hormones that mature and release an egg. For some women, stress can delay ovulation by days or even weeks, and in severe cases, it can temporarily stop ovulation altogether.
Can deep breathing actually help with fertility?
Deep breathing helps by activating the parasympathetic nervous system, lowering cortisol, improving blood flow, and stabilizing the brain–ovary communication loop. It doesn’t replace medical treatment, but it creates a hormonal environment that supports healthy ovulation.
How long does it take for breathing exercises to reduce stress?
Many people feel calmer within minutes, but the hormonal benefits build over weeks. Most research shows meaningful reductions in stress biomarkers after about four to six weeks of consistent practice.
Can stress stop you from getting pregnant even if everything else is normal?
Yes. Even when hormone tests look normal, stress can interfere with ovulation timing, cervical mucus quality, libido, sleep, and uterine blood flow. All these factors influence conception chances month to month.
Does stress affect male fertility too?
Continuous stress may lower testosterone, reduce sperm quality, and increase DNA fragmentation. Stress management matters for both partners, not just women.
Is anxiety during the two-week wait harmful?
Emotional anxiety alone doesn’t prevent implantation, but chronic stress can affect progesterone, sleep, and blood flow. Gentle breathing practices during the two-week wait help keep the nervous system stable and reduce unnecessary tension.
How often should I practice deep breathing for fertility benefits?
Five to ten minutes once or twice a day is enough to make a difference. The key is consistency. Integrating breathing into morning routines, work breaks, or evening wind-down habits helps retrain the nervous system more effectively.
Bringing It All Together: Breath as a Daily Anchor
Deep breathing will not override severe hormonal imbalances, blocked tubes, or significant sperm disorders and it shouldn’t be expected to. But it can reduce nervous system strain, stabilize hormone signals, improve emotional resilience, and soften the physical effects of stress on fertility.
Emma’s experience mirrors what many women discover: when breathing becomes a regular practice, the body begins to unclench. Cycles regulate, sleep improves, digestion steadies, and the emotional load of TTC feels lighter.
The breath is always available free, accessible, and powerful. Each inhale draws in calm; each exhale releases tension and teaches your body that it is safe, supported, and capable.
References:
- Domar AD et al., Fertility and Sterility, 2018 – Stress biomarkers and conception outcomes
- Sgoifo A et al., Endocrine Reviews, 2018 – HPA-axis activation and reproductive suppression
- Pal GK et al., Front Human Neuroscience, 2021 – Vagal activation through slow breathing
- Chan CL et al., J Altern Complement Med, 2016 – Mind-body programs and IVF pregnancy rates
- Goyal M et al., BMC Complement Med Ther, 2020 – Diaphragmatic breathing and cortisol reduction
- Singh S et al., Front Psychology, 2022 – Alternate nostril breathing and cortisol regulation
- Sun H et al., Sleep Health, 2021 – Slow exhalation and improved sleep quality
- Kaur T et al., J Psychosom Obstet Gynaecol, 2020 – Yoga-breath interventions in fertility care
- Dickens LR et al., Psychology & Health, 2021 – Gratitude practice and physiological stress