At gennemgå in vitro-fertilisering (IVF) er ofte komplekst og følelsesladet. Mange faktorer fra hormonbalance til æg- og sædkvalitet påvirker resultatet. I stigende grad undersøger forskere også en mindre kendt faktor, når det handler om fertilitet: det vaginale mikrobiom.
Tidlige undersøgelser tyder på, at de mikroorganismer, der lever i skeden, kan spille en rolle for den reproduktive sundhed og muligvis påvirke implantationen og den tidlige graviditet. Men selv om resultaterne er spændende, er videnskaben stadig under udvikling, og resultaterne er endnu ikke konsistente mellem forskellige studier.
**1. Hvad er det vaginale mikrobiom, og hvorfor kan det have betydning for fertiliteten?
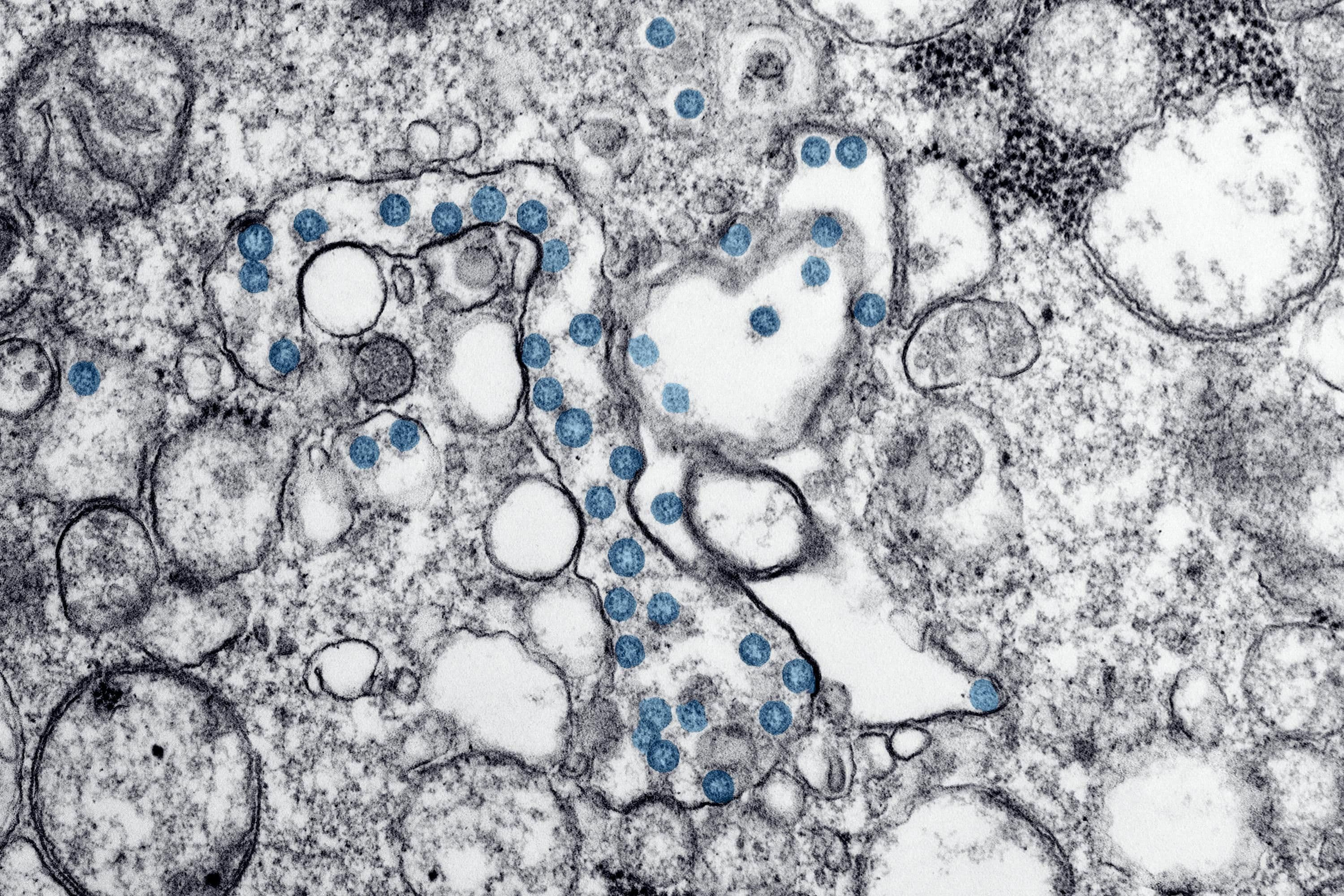
Det vaginale mikrobiom er et samfund af bakterier, svampe og vira, der lever i skeden. I modsætning til tarmen, som nyder godt af mangfoldighed, er det vaginale mikrobiom sundest, når det domineres af Lactobacillus-arter. Disse bakterier hjælper med at opretholde en lav pH-værdi (omkring 4,5), hvilket modvirker skadelige mikrober og understøtter et afbalanceret miljø.
Når denne balance forskydes, kan en tilstand kendt som dysbiose øge inflammationen, hvilket potentielt kan påvirke livmoderhalsslimet, sædoverlevelsen og implantationsbetingelserne.
Sammenhæng med IVF-resultater
Nogle små undersøgelser, som f.eks. en offentliggjort i National Library of Medicine, har observeret, at kvinder med Lactobacillus-dominerende mikrobiomer har en tendens til at have bedre implantations- og levendefødselsrater sammenlignet med dem med mikrobielle ubalancer som Gardnerella vaginalis eller Atopobium vaginae.
Forskerne advarer dog om, at disse sammenhænge ikke beviser årsagssammenhæng, og at der er behov for større, kontrollerede undersøgelser for at bekræfte, om det vaginale mikrobiom kan pålideligt forudsige IVF-resultater.
2. Inflammation og dens potentielle rolle i IVF og graviditet
Sammenhængen mellem inflammation og fertilitet
Inflammation er en normal immunreaktion, men når den bliver kronisk, kan den forstyrre befrugtningen. Noget tyder på, at inflammatoriske markører i livmoderen eller skeden, som f.eks. cytokinerne IL-6 og TNF-alfa, kan være forbundet med implantationsfejl eller tidlig abort (Frontiers in Immunology).
Det er dog uklart, om inflammation direkte forårsager disse resultater eller blot afspejler andre underliggende problemer som infektion eller hormonel ubalance.
Under graviditet
Løbende lavgradig inflammation er blevet forbundet med komplikationer som for tidlig fødsel, præeklampsi og graviditetstab (PubMed, 2022). Håndtering af inflammation gennem afbalanceret ernæring og støtte til mikrobiomet kan hjælpe, selvom det kliniske bevis stadig er begrænset.
3. Livsstilsfaktorer, der kan påvirke det vaginale mikrobiom
Det vaginale mikrobiom reagerer på kost, stress og livsstilsvaner - som alle er særligt relevante under fertilitetsbehandling.
Alkohol og fertilitet
Selv et moderat alkoholindtag kan påvirke hormonbalancen og inflammation. En undersøgelse af IVF-resultater viste, at kvinder, der drak mere end fire alkoholiske drinks om ugen, havde en lavere chance for at blive gravide. Hvis man reducerer eller undgår alkohol mindst et par måneder før IVF, kan det støtte hormonstabiliteten og den generelle reproduktive sundhed.
4. Hormoner, mikrobiom og ægkvalitet: en mulig forbindelse
Hvordan hormoner former vaginale bakterier
Østrogen fremmer glykogenproduktionen i vaginale celler, hvilket giver føde til Lactobacillus, mens progesteron påvirker immunforsvaret og slimhindefunktionen. Når hormonniveauerne svinger på grund af stress, medicin eller kost, kan mikrobiomet ændre sig og potentielt øge risikoen for betændelse.
Ernæring og ægkvalitet
Systemisk inflammation kan også påvirke æggenes sundhed. Kost, der er rig på omega-3-fedtsyrer, antioxidanter og mikronæringsstoffer som CoQ10, zink og C- og E-vitamin, kan hjælpe med at beskytte æg mod oxidativ skade. Selvom evidensen er foreløbig, anses det i vid udstrækning for at være gavnligt at støtte den generelle metaboliske og inflammatoriske sundhed under IVF-forberedelserne.
**5. Kan du teste og forbedre dit vaginale mikrobiom før IVF?
Testmuligheder
Vaginal mikrobiomtestning kan identificere bakteriel balance ved hjælp af en simpel vatpind. Klinikker og hjemmekits kan påvise almindelige ubalancer, der involverer Gardnerella, Ureaplasma eller Candida-arter.
Når man finder en dysbiose, kan man bruge følgende metoder:
- Probiotika (især Lactobacillus crispatus)
- Kostforbedringer med fibre og fermenterede fødevarer
- Stress- og søvnhåndtering
- Medicinsk behandling, hvis der er tale om en infektion
Selv om nogle klinikker tilbyder mikrobiomtestning som en del af vurderingen før IVF, bemærker eksperter, at forskningen stadig er i sin tidlige fase, og at der mangler standardiserede behandlingsretningslinjer.
6. Naturlig understøttelse af vaginal og reproduktiv sundhed
For at opretholde et afbalanceret mikrobiom og stabile hormonniveauer:
- Følg en middelhavskost rig på fibre, sunde fedtstoffer og antioxidanter
- Undgå for meget sukker, forarbejdede fødevarer og alkohol
- Oprethold en sund vægt og regelmæssig motion
- Afstå fra at bruge douches eller parfumerede produkter
- Prioriter søvn og stresshåndtering
Disse trin kan hjælpe med at reducere inflammation og støtte den generelle fertilitet, selv ud over mikrobiomets effekter.
7. AMH-niveauer, inflammation og fertilitetspotentiale
Anti-müllersk hormon (AMH) afspejler æggestokkens reserve og kan også påvirkes af den generelle metaboliske sundhed. Der er ingen dokumenteret måde at øge AMH markant på, men optimering af ernæring og reduktion af inflammation kan understøtte æggestokkenes funktion.
De vigtigste trin omfatter:
- Sikring af tilstrækkeligt D-vitamin, omega-3 og CoQ10.
- Begrænsning af alkohol- og sukkerindtag
- Spise proteinrige fødevarer og anti-inflammatoriske ingredienser som gurkemeje og olivenolie
**8. Kan livsstil forbedre ægkvaliteten? Muligvis.
Selvom alder stadig er den stærkeste faktor for ægkvalitet, tyder forskning på, at ernæring, at holde inflammation under kontrol og indtag af antioxidanter kan forbedre befrugtningspotentialet. For eksempel er antiinflammatoriske kostmønstre blevet sat i forbindelse med bedre embryoudvikling hos kvinder, der gennemgår IVF (Reproductive Medicine).
9. Det vaginale mikrobiom: lovende, men endnu ikke dokumenteret
En 2023 meta-analyse antydede, at vaginal mikrobiel sammensætning kan korrelere med IVF-succes, men beviserne er stadig foreløbige. Selvom mikrobiomvurdering en dag kan blive en del af standard fertilitetsscreening, er det i øjeblikket bedst at betragte det som et nyt forskningsområde snarere end en dokumenteret metode til at forudsige resultater.
Afsluttende tanker: at skabe balance for bedre fertilitet
Dit vaginale mikrobiom er en aktiv del af dit reproduktive system, som interagerer med hormoner, immunitet og inflammation. Selv om der er behov for flere undersøgelser, kan støtte til mikrobiel balance gennem sunde vaner, god ernæring og håndtering af inflammation være med til at skabe det bedst mulige grundlag for undfangelse og graviditet.